| 1) Optimisation of Medical condition and Risk Factors |
A) Improving Control of Diabetes
Diabetic control has to be addressed by an Endocrinologist or a Family Physician who is trained to assess and improve the control of diabetes. A comprehensive screen for the following potential complications should be performed:
- Diabetic Eye Disease
- Diabetic Kidney Disease
- Diabetic Peripheral Neuropathy
Novena Vascular & Varicose Vein Centre has several partner physicians who work closely with us to improve the holistic care of the diabetic patient.
B) Control of Hypertension and Cholesterol
Hypertension (aka High blood pressure) and Hyperlipidemia (aka high cholesterol) are frequently associated with diabetic foot conditions. Control of these conditions with medications, diet control and exercise is essential to prevent stroke and heart disease.
C) Smoking Cessation
Smoking is strongly associated with PVD and heart disease. Continued smoking will also accelerate the progression of atherosclerosis. Novena Vascular & Varicose Vein Centre works with several physicians on dedicated programs that adopt a multi-prong approach to help you stop smoking.
D) Antiplatelet Therapy (Blood Thinners)
Patients who have PVD are at risk of developing other life threatening conditions like Heart Disease and Stroke. All patients with PVD should be started on blood thinners like Aspirin and Plavix which reduce the risk of heart attack and strokes by up to 25%. Patients should consult their Vascular Surgeon on the risk and benefits of blood thinners.
E) Pain Control
Diabetics with or without wounds can experience a lot of pain. It is estimated that 20% of non insulin dependent diabetics will develop Neuropathic pain after 10 years. The pain originates from both the wound as well as damaged nerves. The pain can vary from “pins and needles”, burning sensations, shooting cutting pain, hot/cold sensations in the feet, numbness to the sensation of “walking on marbles”. Novena Vascular & Varicose Centre works with several partner Pain Specialist to help improve the quality of life. Diabetic foot disease doesn’t have to be a painful condition.
F) Nutrition and Pressure relief
For diabetic foot wound to heal, nutrition is paramount. Nutrition allows the body to heal itself. There are also several supplements specially catered to improve the protein balance in the body. There are also several dietary regimes aimed at improving the immunity of the patient.
 
Continued prevention of bed sores and pressure sores is done with dedicated protective devices like this:
|
B) Endovascular Surgery
Endovascular Surgery is a new method of improving the blood supply to the organs. It is commonly known as an “Angioplasty”. It is similar to that done to open blocked blood vessels of the heart. It is a minimally invasive procedure done under Local Anaesthesia under X ray Guidance. It does not involve big incisions and is well tolerated with minimal pain.
The Endovascular Surgeons at Novena Vascular & Varicose Vein Centre are highly trained in performing Endovascular Surgery. They are Medical Advisors and Regional Proctors to several Endovascular Companies like Medtronic, Abbott, Covidien, Cordis, Biotronik and Straub Medical.
The benefit of Endovascular Procedures are:
- It can be performed even with heart conditions as it does not require General Anaesthetic and is lower in risk as compared to a bypass
- It is a quick procedure generally lasting between 1-3 hours
- It has good short term results
- It is minimally invasive with less pain during and after the procedure with almost no cuts, just an injection
- It is relatively affordable
- It can be repeated with minimum risk if necessary
- It can open multiple blood vessels
What happens during the procedure?
 Before the insertion, the nurse will clean your skin and shave any hair in the immediate area. This is done to reduce your risk of infection. Your doctor numbs your skin with local anaesthesia and then makes a small cut or puncture to reach the artery below. Although you may be given some mild sedation, your doctor will usually want you to stay alert to follow instructions and describe your sensations during the procedure. Before the insertion, the nurse will clean your skin and shave any hair in the immediate area. This is done to reduce your risk of infection. Your doctor numbs your skin with local anaesthesia and then makes a small cut or puncture to reach the artery below. Although you may be given some mild sedation, your doctor will usually want you to stay alert to follow instructions and describe your sensations during the procedure.
The doctor then inserts a thin hollow needle into an artery or a vein in the groin, elbow, or in the armpit. Through this needle under X-ray, a wire followed by a very thin plastic tube (catheter) is advanced to the narrowed vessel. A dye(contrast) is then injected into your arteries to visualise the blockage. This is called an Angiogram.
During this time, you may experience a brief warm sensation. This is normal. You should try to lie very still during the injection to prevent blurring of the pictures. During the test, we may ask you to hold your breath for about 5 to 15 seconds.
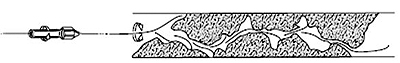
The wire is manipulated to cross the narrowed segment of artery under X-ray:
Depending on circumstances, the following therapies can be used to open the blockage:
i) Balloon Angioplasty
Under X-ray, a deflated balloon is positioned across the narrowing or blockage. The balloon is inflated to press the plaque against the vessel wall and this may last between 1 to 5 minutes. Occasionally, this may be repeated. Your artery may stretch and your blood flow through the artery stops when the balloon is pushing your artery open. This may cause pain. However, the pain should go away when your doctor deflates the balloon and normal blood flow resumes. Do tell your doctor if you experience any symptoms during angioplasty.
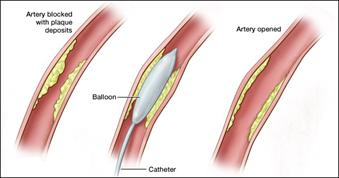
The balloon is completely removed after the procedure.
Drug Eluting Balloons may also be used to improve the durability of angioplasty. These balloons are coated with very low doses of chemotherapy agents to prevent re-scarring/re-narrowing that frequently occurs after angioplasty.
ii) Stent
 A stent is a tiny mesh tube that looks like a small spring is an inert metal which is expanded to act like a scaffolding to keep the blood vessel wide open . If the stent is required, it is usually placed easily at the same time after suboptimal results after balloon angioplasty. The stent remains in place to support the walls of your artery. Your artery walls grow over the stent, preventing it from moving. Although stents help prop open your arteries, scar tissue sometimes can eventually form around stents and cause restenosis or re-blockage A stent is a tiny mesh tube that looks like a small spring is an inert metal which is expanded to act like a scaffolding to keep the blood vessel wide open . If the stent is required, it is usually placed easily at the same time after suboptimal results after balloon angioplasty. The stent remains in place to support the walls of your artery. Your artery walls grow over the stent, preventing it from moving. Although stents help prop open your arteries, scar tissue sometimes can eventually form around stents and cause restenosis or re-blockage
A new type of stent is coated with drugs, the Drug Eluting Stent. These drugs may help prevent scar tissue from forming inside a stent. Studies have shown that these new stents may be more likely to prevent restenosis than ordinary, non-coated stents.
There are also ultra-flexible stents:
New Generation Stents

SUPERA Stents


iii) Other forms of treatment
Other forms of treatment that may be used / include but are not limited to:
- a cutting device to remove the plaque or debris that is causing the blockage (atherectomy)
Shave Off The Plague

- a rotary instrument to remove blood clots (percutaneous thrombectomy)

Atheretomy of Left SFA

‘Clot busters’ which are used to dissolve blood clots (thrombolysis)
Bioabsorbable stents. These are new generation stents which are completely absorbed after 2 years. They are also coated with a medication to delay re-narrowing. The benefit is that there is no permanent metallic implant left in the artery.
Drug Coated Bioabsorbable Stents

The most common therapy is Angioplasty with or without supplementary Stenting.
During all these procedures, blood thinners will be used to prevent clots in your arteries/veins. Other medications may also be used to relax your blood vessels.
At the end of the procedure, dye is again injected through the catheter to see the results of the therapy. Further treatment during the same setting or at another time may be required to achieve a satisfactory result.
A typical procedure normally lasts 2 to 3 hours. However, in complex cases, the procedure may stretch longer.
At the end of the procedure, the doctor will remove the wires and balloons from the injection site. He may do the following:
Apply a compress on the injection site for 10-15 minutes which may cause some discomfort. After compression, you must lie still in a flat bed for 6-24 hours to prevent bleeding at the injection site.
He may use a device to artificially close the injection hole in the which will allow you to move around after 2 hours.
What happens after the procedure?
Usually, you need to stay in bed for 2 to 24 hours after your angioplasty depending whether a closure device was used. You will frequently be required to rest in bed.
During this time, you will be closely monitored for any complications by your doctor and nurses.
If you notice any unusual symptoms after your procedure, you should tell your doctor or nurse immediately. These symptoms include fever, shortness of breath, leg or back pain that lingers or gets worse, an arm or a leg that turns blue or feels cold, and bleeding, swelling, pain or numbness around your injection site.
After the procedure, you should drink plenty of water for 2 days to help flush the contrast dye out of your body. You can usually shower 24 hours after your procedure.
Your doctor will prescribe aspirin or other medications that thin your blood. These medications will help prevent clots from forming on your stent. Your doctor will usually see you the next day to explain the results and make sure you have not developed any complications.
It is important that you STOP SMOKING and take all your prescribed medications to prevent the blockages from reforming i.e. restenosis. This may happen very soon in some cases. Your doctor will advise you accordingly.
You may be scheduled for more ultrasound scans after the procedure. This is to detect restenosis. Depending on circumstances, your doctor may recommend a repeat angioplasty.
Carbon Dioxide Angioplasty is a new method of performing an angioplasty without the use of conventional Dye. In patients with kidney disorders, excessive dye usage during angioplasty may worsen renal function. CO2 angioplasty does not require conventional dye but uses the gas a a form of dye. It is safe and does not put the kidney at risk.
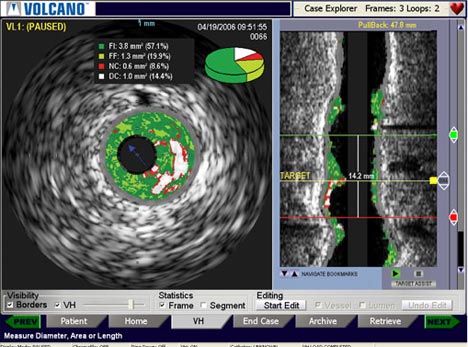
Intravascular Ultrasound (IVUS) is occasionally employed to visualize the blood vessel inside out. An ultrasound probe is inserted into the blood vessel to visualize the narrowing. It supplements existing X Ray guidance.
C) Hybrid Open Vascular and Endovascular Surgery
Hybrid procedures involved a combining Open Surgery with Endovascular Procedures. This combines Open Surgery with Angioplasty done under X ray guidance in a Hybrid Operating Room. It combines the benefits of both open and endovascular surgery.
Remote Endarterectomy is a typical hybrid procedure that combines open surgery and Endovascular techniques. Through a medium sized incision in the groin, the plaque in the artery of the thigh is cored out.
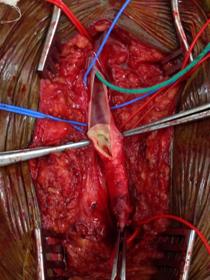 

| 3) Removal of Unhealthy Tissue and Control of Infection |
For a Diabetic foot wound to heal, it is important to:
- Remove all unhealthy tissue and drainage of deep seated pus
- Treat underlying infection by giving appropriately selected antibiotics
The removal of unhealthy tissue and drainage of underlying pus can be done by:
- Surgical excision under regional or general anaesthesia.
This can be painful and is best done in the Operating Theatre in clean and aseptic conditions. Newer techniques of removing unhealthy tissue like Versajet Hydrosurgery can be done. This helps to remove unhealthy tissue whilst preserving viable tissue.
Novena Vascular & Varicose Vein Centre works with partner anaesthetist who specialize in Regional Anaesthesia (focal anaesthesia given to numb certain nerves) which is safer for patients with multiple medical problems.
Debridement (removal of unhealthy tissue) in the clinic. This is generally reserved for minor debridements and can generally be achieved with minimal pain.
Local anaesthetic is commonly given and this is generally well tolerated. Debridements in the clinic are done in the treatment / Podiatry Room under sterile conditions.
The podiatry and treatment room

At Novena Vascular & Varicose Vein Centre, we have a fully equipped Podiatry and Treatment Room.
As the wound heals, patients may require repeat debridements/operations to clean the wound. Under Regional Anaesthesia, this can be safely done.
Treatment of Infection:
After the drainage of underlying infection and removal of unhealthy tissue, it is crucial to treat the infection with antibiotics. Guided by tests sent to identify the specific bacteria, we can start the appropriate antibiotics.
This is usually given intravenously (i.e. IV) through a small plastic needle in the vein. Novena Vascular works with partner specialist who provide and Outpatient Home or Clinic based Antibiotic Service for even greater convenience.
4) Wound Care & Dressings |
Wound care is essential to allow the body to heal itself. It is an ongoing process that requires minor wound debridements (removal of unhealthy tissue) as well as wound dressings. This provides and optimum environment for the growth of healthy tissue.
Wound debridements can be done in the clinic using sterile equipment. An ultrasonic machine can also be used to debride the wound. Click on the link below to see video:
Novena Vascular & Varicose Vein Centre has a wide range of wound dressings available. These include silver based dressings, collagen based dressings Negative Pressure Therapy. Wounds require different dressings at different stages of wound healing.
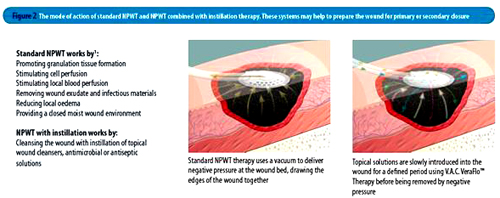
One of the most effective dressings in Diabetic Foot Wounds is the VAC dressing. It is essentially a dressing using Negative Pressure i.e. Suction to encourage wound healing.
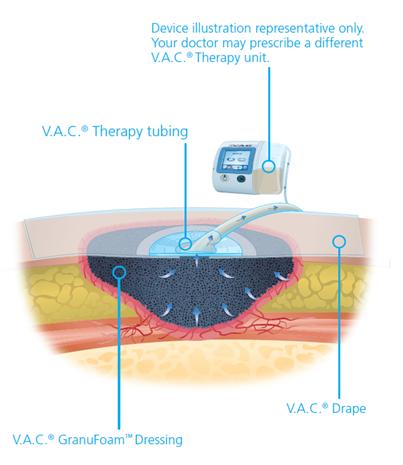
The benefits of VAC Therapy are:
- Removes infectious material and fluids from wound
- Provides a waterproof environment and prevents contamination from the environment
- Improves blood flow and encourages healthy tissue to form and grow
- Reduces swelling
- Convenient portable light weight system with a long battery life
- Does not require daily change of dressing
- Reduces odour
Learn about patients experiences with VAC therapy
Download the Patient Information Brochure
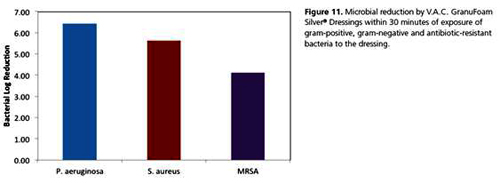
VAC dressing can also be treated with Silver based compound. Silver used to reduce the infection on the surface of the wound. The diagram below shows the reduction of bacterial after 30 minutes of exposure to Silver based VAC:
A new form of VAC called UltaVac allows continued cleansing and irrigation of the wound with antibacterial solution whilst the wound is subjected to intermittent suction. Programmed periods of irrigation with fluid are alternated with suction
Click on the link for an article on UltaVac
Our doctors were the pioneers in the application of this revolutionary new product. They are also Regional Consultants for KCI Medical, the makers of VAC.
|


